Discover more from Long COVID: Insights from a journey back to wellness
I got COVID-19 in March 2020. As a scientist focused on immunology, I was better prepared than many, but it was clear from the onset that this was not like any viral infection that I had ever had. While hospitalization was avoided, the symptoms, especially brain fog, fatigue, and digestive disorders overshadowed my life for more than two years.
After months of coping, trying the treatments recommended by my providers, and hoping that the symptoms would eventually fade away, I realized that I needed a new strategy. It seemed reasonable that between my training and years of experience in immunology, along with access to insightful colleagues and high-quality research, that I could uncover more about the underlying issues I was experiencing with long COVID.
In my research, mitochondrial dysfunction emerged repeatedly as a cause of many COVID-19 symptoms. It made sense to me. Mitochondria are tiny energy factories found in every cell of every tissue and organ in the body and I knew that they could be damaged by inflammation. COVID-19 or other long-term issues could be causing inflammation that was in turn, continuing to damage vulnerable mitochondria.
So, if inflammation was a factor keeping me sick with Long COVID, I needed to uncover what factors were causing the inflammation in my body.
Since my Long COVID symptoms of chronic diarrhea and acid reflux were not responding to medications recommended by my doctors, a trusted colleague suggested that I look at my diet. I bristled at the idea that my diet might be playing a role. It had never previously been a problem. After all, I was eating a diet rich in fiber, fruits, grains, and vegetables. We bought high-quality milk, meat, poultry, and eggs. What could possibly be wrong with my diet?
I turned to research to dig deeper and to uncover how the food I was consuming, despite its quality, may be a factor in the inflammation present in my body. If I was going to determine what might be causing me problems, I needed to eat non-inflammatory foods for long enough to uncover what was causing the issues, which in turn could reset my immune responses and support the healthy microbes that partner with our bodies to support good health. I knew that there were foods that are highly inflammatory and others that are anti-inflammatory. So, based on research reported by established scientists, I began with a two-week trial to see if changing my diet could make a difference.
My strategy was to protect my mitochondria from a perpetual cycle of damaging inflammation and to nurture them back to optimal function.
In those first two weeks, I eliminated the following foods from my diet:
· All processed foods including meats and condiments like mayonnaise, soy sauce, prepared salad dressings, etc.
· All foods containing sugar, honey, maple syrup, and artificial sweeteners
· All gluten-containing foods (all foods containing any form of wheat, barley, oats and rye)
· Most other grains including corn, buckwheat, quinoa, rice, and spelt
· All nightshade vegetables including tomatoes, potatoes, peppers, and eggplant
· All processed vegetable oils
· All cow’s milk and cow’s milk dairy products
· Eggs and products containing eggs
· Beef, bison, lamb and pork
· Nuts
· All legumes, in any form, including soy, peas, peanuts, beans, lentils, and food that contain them.
In short, for the test period, I eliminated foods that are known to cause inflammatory responses in some humans even if they had not been a problem for me pre-COVID.
My dietary approach had three objectives:
· Begin the process of determining which foods, if any, were inflammatory to my system.
· Begin the process of resetting my immune system responses to foods that had become inflammatory to my system.
· Support my gut microbiome to populate with beneficial bacteria.
Within a few days, many of my most serious symptoms began to improve. My brain fog began to lift. The intensity and frequency of my fatigue decreased. Acid reflux stopped. Bloating and abdominal pain disappeared. Diarrhea symptoms began to improve.
You might be asking, what the heck did I eat during those critical two weeks?
My diet focused on eating cruciferous (vegetables in the cabbage family, like broccoli, Brussel sprouts and cauliflower) and green leafy vegetables, some root vegetables (like beets, carrots, and radishes), avocado and small amounts of other fruits that supported digestion, and small servings of pasture-raised chicken and ocean-caught fish. I cooked and dressed my meals with cooked mushrooms, olives, avocado, and with extra virgin olive oil and refined organic coconut cooking oil. A squeeze of fresh lemon juice or unpasteurized organic apple cider vinegar provided the tang to balance the flavor. In those first two weeks, I also switched to goat’s milk products, rather than consume cow’s milk dairy.
To the extent possible, I seek organic, pesticide free foods, pasture-raised animal and poultry products and ocean-caught fish. Yes, they can be expensive and hard to find, but in contrast to medical costs, loss of employment, and suffering, I find them to be a bargain.
Here’s a list of plain and simple foods that proved to be safe and effective to address my symptoms in that early phase of testing. Note that most of these foods contain nutrients that are specifically anti-inflammatory, such as polyphenols, omega-3 fatty acids, medium chain fatty acids, and factors that stimulate liver and kidney enzymes (that remove toxins (xenobiotic) from the body. (If the list sounds restrictive, remember that I did this original testing phase for two weeks, not the rest of my life.)
· Broccoli, cauliflower, Brussel sprouts, Bok choi (and any other member of the cruciferous vegetable family)
· Lots of green leafy vegetables such as lettuce, kale, arugula, chard, spinach, beet and turnip greens (I enjoy these raw in salads or sauteed with onions and garlic.)
· Celery, parsley, basil, garlic, onions, scallions, leeks, chives
· Cooked mushrooms, especially shatake and portobello mushrooms
· Olives
· Extra virgin olive oil, avocado oil, refined liquid coconut cooking oil
· Unpasteurized organic apple cider vinegar or balsamic vinegar, lemon and lemon juice
· Very small servings of papaya, mango, avocado, and bananas, all of which aid digestion
· Small servings of sweet potato, turnips, carrots
· Small servings of pasture-raised chicken (sometimes difficult to find) and ocean-caught fish, especially salmon, mackerel, sardines, herring, or anchovies
· Small servings of goat’s milk and goat’s milk cheese, yogurt, or other goat’s milk products.
· One small serving of very dark chocolate each day
· All of the coffee or tea that I wanted to drink
· Several glasses of water per day.
· Miso used to make a soup base and/or as a flavoring when cooking
During this test, I began to understand that foods that had previously been safe and important mainstays of my diet were causing at least some of my problems. And it wasn’t just about the nutrients for my system. My encounter with COVID had apparently changed my microbiome (the bacteria in my gut). I needed to provide that dwindled population with foods that fostered healthy gut microbes (microbiota) to restore my gut health. (I will address the relationship between gut microbes and intestinal immune cell responses in a future post.) A healthy gut microbiome is, in part, supported by consumption of leafy green vegetables and by not consuming sugars and foods laced with chemicals that can shift the balance away from beneficial microbes.
There was a balancing act taking place in my system. I couldn’t restore my health until I reduced the overall inflammation that was damaging my mitochondria. Food was the first factor that helped me peel a layer back to better understand the impact that long COVID was having on my systems. While improvements were significant after the first two weeks, my overall health and vitality were not back to my pre-COVID state. I knew I needed to continue my research to further uncover ways to improve.
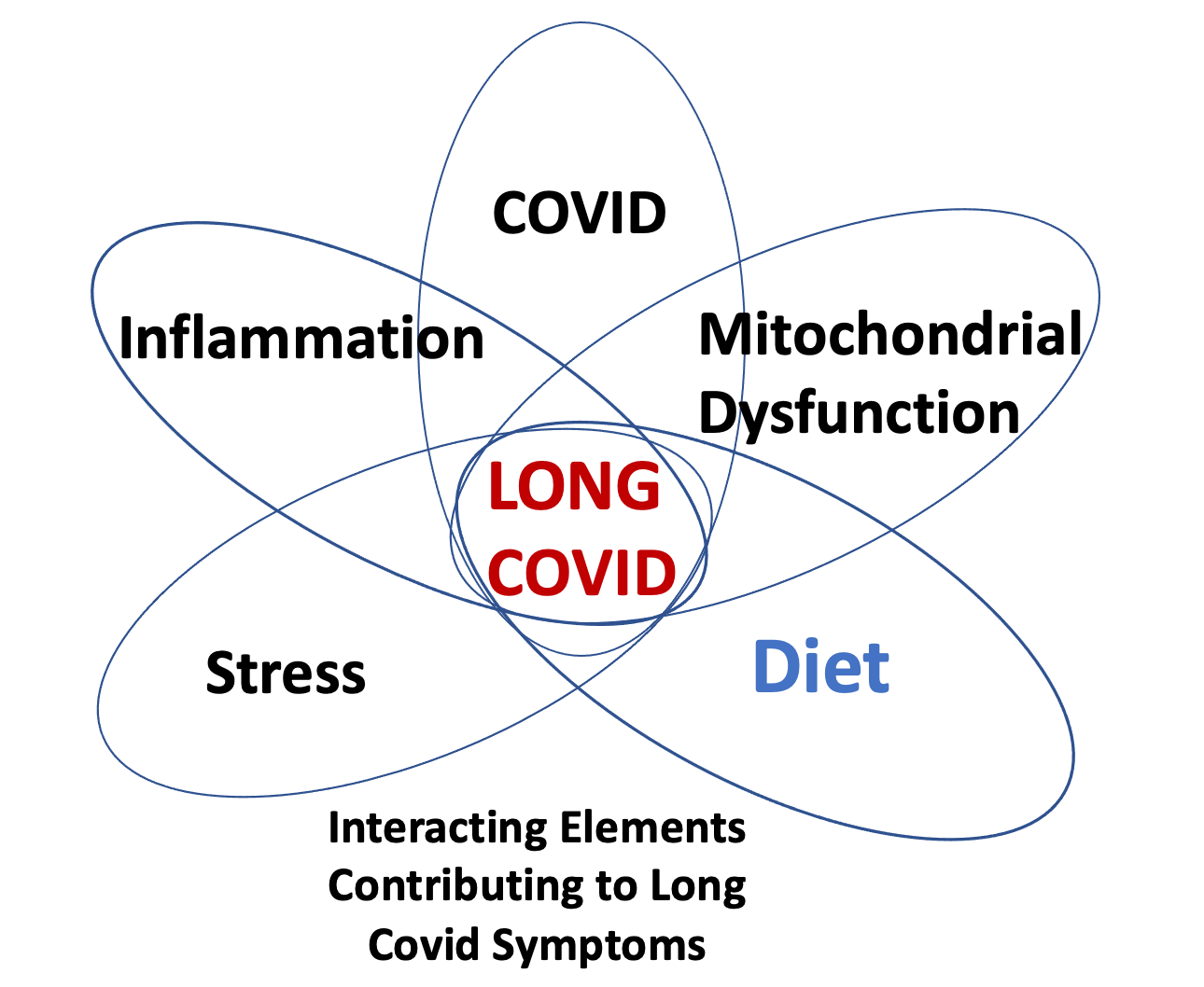
If you reflect on the diagram at the top of the page, you will see overlapping influences, all of which, I believe, are necessary for Long COVID symptoms to be present and ongoing. Diet for me was part of the problem and switching to eating non-inflammatory foods was a key part of the solution.
There is much more to say about diet including how I determined which foods were problematic for me and how I dealt with that information. My next post will also include discussion of the supplements that I learned that I needed to nurture my mitochondria.
For those who follow this blog as scientists, medical providers, employers, and decision makers involved in policy, please consider the implications of diet and the availability of foods to patients, employees, and constituents. Your awareness and engagement of these issues can change the impact of Long COVID on individuals and society.
Selected Resources
COVID-19: What we eat matters all the more now.
Gundry SR, Solimene C. The plant paradox. Tantor Media, Incorporated; 2017.
Integrative medicine considerations for convalescence from mild-to-moderate COVID-19 disease
Plant lectins activate the NLRP3 Inflammasome to promote inflammatory disorders
Subscribe to Long COVID: Insights from a journey back to wellness
Mardi Crane-Godreau, PHD, Long Covid recovery: Dr. Crane-Godreau's articles guide the reader toward wellness, including scientific research and notes from her personal experience.














This was a great article. Thank you for your research and for sharing what worked well for you. I am working with a medical group based in Montpelier VT that is looking specifically at long COVID in neurodivergent populations and trying to come up with some guidance to help their patients. Many of these people had some autoimmune conditions prior to long COVID symptoms but the long COVID made it significantly worse and triggered other autoimmune disorders. How much are you looking into the types of physiologic profiles that seem to struggle more with long COVID and would you be willing to talk with the executive director of All Brains Belong about your findings?
Thank you Dr Crane! Your recommendations about specific foods to avoid are very helpful!