Discover more from Long COVID: Insights from a journey back to wellness
In this post I review the process of sorting out what foods could best support my recovery and provide a list of supplements that I believe have been critical in helping me turn the corner on Long COVID. In my case, ruling out causes of inflammation proved to be a critical pivot point in my recovery.
As mentioned below, “Determining which foods might be inflammatory to my system was a challenge but given the alternative of remaining locked into brain fog, fatigue and many other unpleasant Long COVID symptoms, I decided on and then stuck with the process of testing.”
Two years of Long COVID was at times like swimming through pea soup. As a scientist trained in immunology, I was both frustrated and curious about my illness. Why was I on a downhill slope and getting sicker? It was at this point that a trusted colleague suggested that I look at my diet.
In a previous post, I described how I began testing to determine which foods, if any, might be influencing my health.
There is strong evidence that when the SARS-CoV-2 Virus enters cells, that it homes to organelles like the mitochondria and endoplasmic reticulum. Mitochondria are energy factories for all body functions. They also play an important innate immune system role, detecting and disabling viruses. Damage to mitochondria by the virus results in mitochondrial dysfunction. Symptoms like muscle weakness and brain fog are consistent with mitochondrial dysfunction. My objective in testing the role of food was to find nourishment that would not damage mitochondria through inflammation and would support nurturing them back to optimal function.
Based on established science, I took a two-week vacation from eating foods that I will call “prime suspects”. I had to stop eating suspected/potentially inflammatory foods for a brief time to determine the culprits in my Long COVID symptoms. Within about 3 days of my food vacation, I knew that there was a strong connection. Many of my most serious problems improved. The depth and duration of my fatigue decreased. My brain fog began to lift. Acid reflux and bloating stopped. The never-ending diarrhea began to decrease. While I knew there was still a long way to go, it felt like there was light at the end of the tunnel.
There were 3 objectives in taking a vacation from potentially inflammatory foods and building a diet around anti-inflammatory and health-promoting foods:
· Begin the process of determining which foods, if any, were inflammatory to my system and which foods might be involved in the ongoing (chronic) nature of Long COVID.
· Begin the process of resetting immune system responses to foods that had become inflammatory to my system.
· Support my gut microbiome to populate with beneficial bacteria.
Determining which foods might be inflammatory to my system was a challenge but given the alternative of remaining locked into brain fog, fatigue and many other unpleasant Long COVID symptoms, I decided on and then stuck with the process of testing.
I removed many prime suspects from my diet but, you might be wondering what did I eat during this two-week test? My diet was varied and comprised of organically raised leafy green vegetables including various types of lettuce, kale, parsley and celery. I ate cruciferous vegetables like broccoli, cauliflower, arugula, and cabbages. I enjoyed avocadoes, mushrooms, onions and garlic, beneficial fats like olive oil, and small servings of pastured-chicken and fresh or frozen ocean-caught cold-water fish.
Beneficial gut microbes flourish when the fiber and nutrients from green leafy vegetables are present. Inflammatory microbes are starved by eliminating sugars and certain food contaminants from the diet. Breakfast, lunch, dinner, and snacks came from these core foods.
The foods that I eliminated from my diet during my two-week test fit into various categories that fit my understanding and previous history with food sensitivities. Briefly, here are the groups that I was trying to test:
· Eggs
· Cow’s milk for its casein proteins and the milk sugar lactose.
· Gluten, gliadins, and related proteins found in wheat, oats, barley and rye.
· Lectins associated with all legumes (beans, peas, lentils, etc.), most grains, and many fruits and vegetables.
· Nuts
· Beef to rule out any allergy associated with the carbohydrate galactose-α-1,3-galactose (alpha-Gal).
· While the role of nightshade vegetables as sources of inflammation is controversial, I wanted to test this group as well.
· Eliminating sugar was to support changes in my gut microbes and to protect my digestive tract against undigested sugars that can be involved in some forms of diarrhea.
At the end of two weeks, I had seen enough improvement to suggest some of the foods that I had been eating prior to the food vacation test period were contributing to the inflammation in my system. One or more were perpetuating my Long COVID symptoms. The next step was to re-introduce foods. I needed to find out which foods were the culprits and, which ones might be safe during my healing process.
Re-introducing foods can be an adventure. Which food should be tested first? My first choice was eggs. I was pretty sure that eggs were not a cause of inflammation for my body. I gave it a 3-day test and had no problems. My next trail was to test cow’s milk. That did not go so well; I experienced bloating and other digestive issues. It took me a couple of weeks of trial and error to discover that the culprit was likely A1 casein, a protein found in most cow’s milk. Casein A2 comes from a subset of cows and is easier to digest. (A2/A2 milk is commercially available.) When I experimented, restricting my cow’s milk to only the A2 form, digestive issues were no longer a problem. In contrast to cow’s milk, goat’s milk remained easy to digest and was a nutritionally sound choice.
Food sensitivities and allergies can come from several different causes. The enzymes needed to safely digest food can vary based on a person’s genetic background. Sensitivities can also develop due to changes in which of our genes are expressed. For example, some children may easily digest milk early in life but as adults, find that milk and milk products may be difficult to digest. Gluten sensitivity is another genetically driven problem. If the enzyme needed to digest it are not present, gluten can harm the lining of the digestive tract leading to a host of other problems.
Another cause of food sensitivities can be the development of leaky (permeable) gut when food molecules cross from the intestines and encounter immune system cells. A good deal of research over the last decade has begun to show how important a healthy microbial biome (the microbes that live in the gut) is to lessen (temper) the extremes of many food sensitivities. A healthy diet supports healthy gut microbes and in turn can reduce inflammation in our system, ultimately supporting mitochondria repair and helping us heal from illnesses like long COVID.
A great gift that I gave myself was a modern pressure cooker. Many foods are high in lectins, naturally occurring plant proteins that can be difficult to digest. Some lectins have been associated with inflammation. Many high lectin foods can be made more digestible by cooking them in a pressure cooker. More details on food preparations and some delicious choices in the next blog post.
*********** If you would like to comment or to like this post, you need to be an active subscriber. Subscriptions are free. Your input is appreciated. Thank you! *********
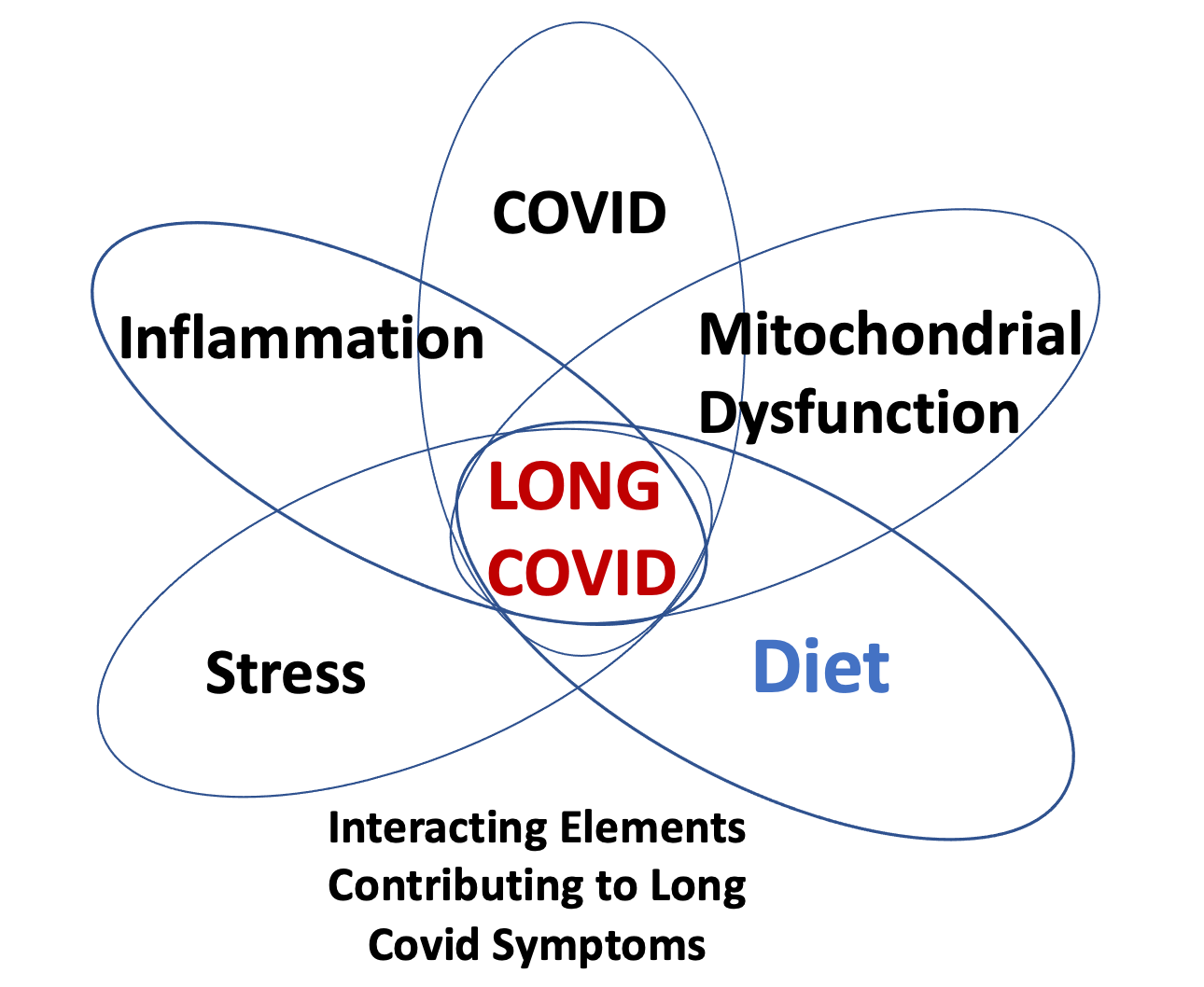
The diagram at the top of the page, illustrates that both diet and inflammation overlap mitochondrial dysfunction. My strategy to recover from Long COVID involved removing inflammation while nurturing the mitochondria, supporting return to normal function. I did this with nutrients that are known to be needed by these tiny energy factories. In addition to the diet described above, here is a list of the nutrients that I incorporated into my daily regimen to specifically nurture my mitochondria and to protect them against ongoing potential sources of inflammation:
· All of the B-complex vitamins: Stand-alone B-Complex supplements are available, or these vitamins can be found in many high-quality multi-vitamins. They include thiamine, riboflavin, niacin (nicotinic acid), niacinamide (nicotinamide), pyridoxine, biotin, pantothenic acid, folic acid, and vitamin B12. B-Complex vitamins are necessary for production of energy (ATP) by mitochondria to support body functions.
· Co-Enzyme Q-10 which is necessary for production of energy (ATP) by mitochondria to support body functions.
· Vitamins C and E. Vitamins C and E are needed for production of energy (ATP) by mitochondria to support body functions. Vitamin C is useful to quench reactive oxygen species (ROS).
· Vitamin D is a hormone (transcription factor) that regulates hundreds of body processes. It plays a vital role in managing the immune system, including fostering the ability to identify the nature of microbial threats. It is also protective against immune system excesses such as those known as a cytokine storm.
· Trace minerals selenium and zinc. Selenium is needed for production of ATP by mitochondria. Zinc plays a role in important enzymatic reactions within the body including healing. Both can be found in high-quality multi-vitamin supplements that provide safe levels of both.
· Fish oil high in Omega 3 fatty acids. Fish oil contains anti-inflammatory properties.
· Melatonin. Here melatonin is involved in mitochondrial production of energy, not solely as a sleep aide. I take a relatively small dose at bedtime to support both needs.
· Caffeine helps to support ATP production, so I happily enjoy my coffee and tea.
· Mitochondria also need fuel to make ATP and to self-repair. While the common fuel used by mitochondria is glucose, I consume small amounts of medium chain fatty acids (MCT). MCT provides a fuel needed to make ketones which are more easily processed by mitochondria than glucose. Like my schedule for vitamins D & C, I spread out consumption during the day. I include a teaspoon of organic liquid refined coconut cooking oil with each meal. (This is a pure form of MCT, not the same product as the solid form of coconut oil which contains high levels of long chain fatty acids.)
There is far more to say about the process of food selection and how I determined safe from inflammatory foods. More in the next post.
Please post your comments and questions. You need to add your email to ‘subscribe’ and to be part of the conversation.
TECHNICAL RESOURCES
Omega-3 fatty acids, cardiovascular risk, and the resolution of inflammation
Plant Lectins Activate the NLRP3 Inflammasome to Promote Inflammatory Disorders















Are you taking magnesium? How much? What kind?
Important information, easily digestible.